Bitter Pills
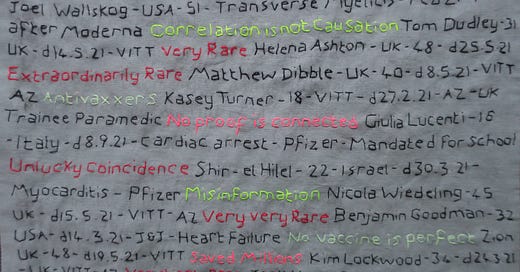
When a person or loved one has sustained life-changing injuries or been killed by a novel prophylactic pharmaceutical product, sold to them as not only safe and effective but essential, it must be very hard to cope with the senselessness of it all. For these people, there will be many bitter pills to swallow in the months and years to come.
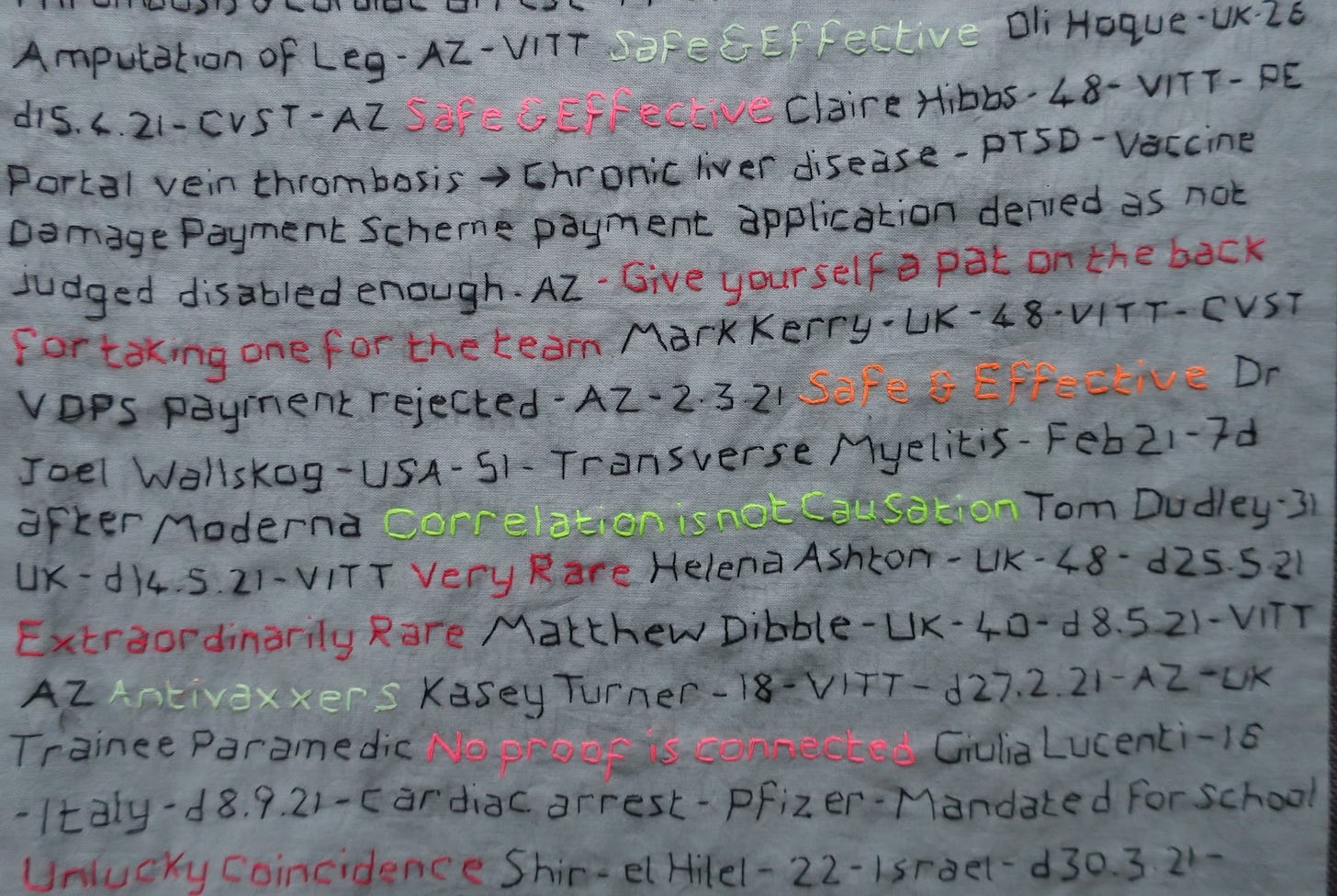
In the UK, the vaccine injured and bereaved are reliant on the Vaccine Damages Payment Act Scheme (VDPS) for compensation. The VDPS may authorise a one off payment of up to £120,000 to anyone permanently disabled or harmed as a result of a listed vaccination. It is tough to prove causality and in the 39 years prior to the pandemic, only 936 claims for a vaccine damage payment had been successful. Those seeking compensation have described the VDPS process as clunky, complicated and bewildering and have felt ‘left in the dark, without any support’.
The UK made its first Covid vaccine compensation payout in June 2022, to the partner of a 48 year old man whose death in May 2021 was caused by the Oxford-AstraZeneca vaccine.
By June 2023, more than 4000 Covid-19 VDPS applications had been made, only 96 of which had been approved. Even so, this already equated to over £11.5m in vaccine damages. By November 2023, 8363 claims had been submitted, of which only 157 were successful; 55 deaths were confirmed as causally linked; 3982 claims had been rejected and 278 were deemed not injured enough to qualify. By March 2024 the number of claims had risen to 9519, with only an extra 6 qualifying for compensation in the preceding four months. Fewer than five of these successful claims were for Pfizer and Moderna.
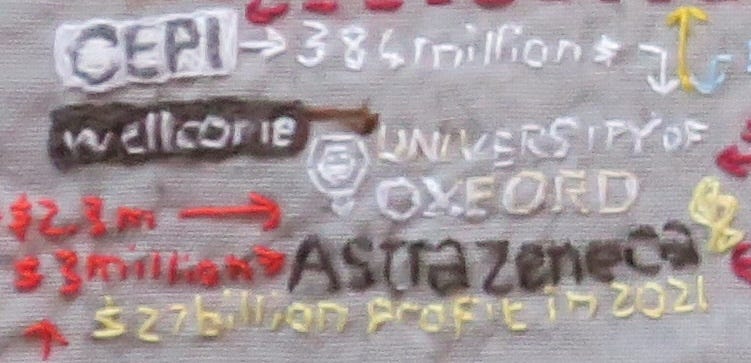
Jefferson and Heneghan have covered this subject in a Trust The Evidence substack post on 8 April 2024, drawing attention to a revealing list of conditions where causality had been accepted but which had failed to meet the 60% disablement threshold for compensation:
The NHS has admitted that "it will take longer before it can be determined if an individual’s claim meets the first legal test of causation” as links between the vaccines and side effects are still being investigated. By March 2024, 394 VDPS claimants had been waiting over 12 months for an outcome, of whom 57 had waited over 2 years without a decision.
To add insult to injury, unsuccessful claimants may have strong evidence for vaccine injury, but if they fail to meet the arbitrary ’60% disabled’ threshold required to receive a payout they get nothing, even when causality is beyond doubt.
Causality
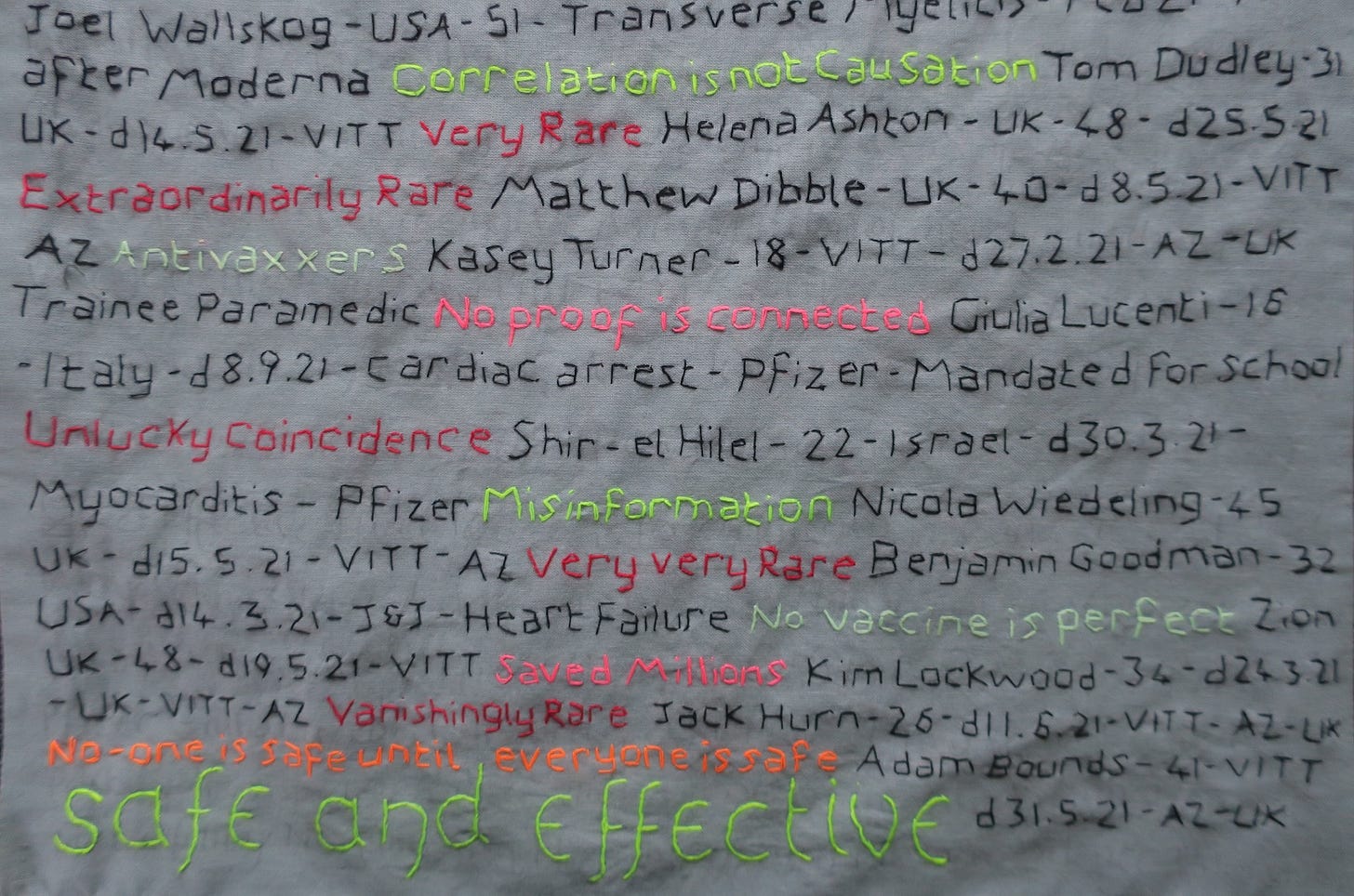
The Covid-19 vaccines were approved based on short term trials that weren’t powered to detect rarer harms and, despite claims to the contrary, without long term safety data we simply cannot know about long term safety of any drug or treatment.
If you cannot establish causality you will not be compensated. If your healthcare provider refuses even to accept the possibility of causality, you will have to fight harder. Some medical professionals have reassured patients that a temporally linked condition is coincidental or cannot be due to the vaccine, because it is not a known or recognised risk. The sticky issue of causality should remain a concern, given the apparent overwhelming dissonance within the medical profession when it comes to discussing potential vaccine injury and our flawed systems for detecting harm.
Not all adverse events from new drugs will be immediately apparent and drug companies are notorious for failing to quickly report serious and unexpected potential side effects from drug trials and post-marketing surveillance. We have seen examples of this kind of behaviour in independent analysis of the released Pfizer and Moderna trial data. Since 2002, Pfizer has been forced to pay $10,948,368,523 in penalties for regulatory violations and other forms of misconduct, including $5,636,840,000 for drug or medical equipment safety violations.
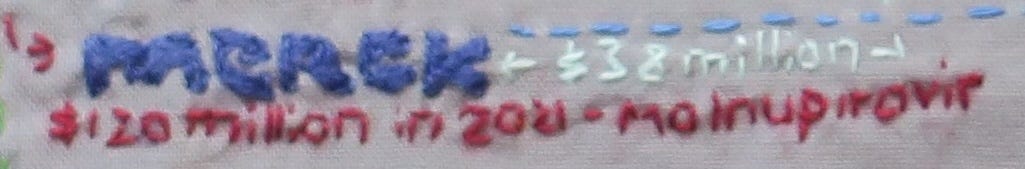
The Vioxx scandal shows us that even a doubling of cardiovascular risk can be missed for years, obscured by the background signal. Vioxx was withdrawn from the worldwide market in 2004, after it was shown to increase cardiovascular risk. It has since been estimated that 88000 Americans had heart attacks from taking Vioxx, and 38000 of these people died.
It took 5 years for the cardiac risks of Vioxx to become firmly established but in his book ‘Deadly Medicine and Organised Crime - How big pharma has corrupted healthcare’ (2013), Peter Gotzsche describes how the evidence was already there in Merck’s clinical trials - two trials showed increased cardiovascular events, but they chose not to publish the results of one of the trials which had ended in 1999 (study 090) until 2006, two years after Vioxx had been withdrawn from the market. In the VIGOR trial, data were manipulated, patients with heart attacks excluded from analyses and one cardiac death deliberately miscoded as something else. Merck selected an earlier cut-off date for the thrombotic events than for the gastrointestinal events, which led to erroneous conclusions about cardiovascular safety. Conflicted officials within the FDA allegedly threatened, intimidated, smeared and discredited whistleblowers and interfered with publication of safety concerns.
It is worrying to hear emerging reports of the same sort of issues affecting the Covid-19 trials.
Protocol Deviations
In a BMJ Rapid Response (2023), retired UK GP Peter Selley points out potential financial disincentives for admitting causation in clinical trials. If drug companies agree that an adverse event is directly due to administration of their product, they not only acknowledge the association between their product and the adverse reaction, but are also potentially liable for ensuing medical bills arising from that adverse event. Of the 21,926 adult participants to receive Pfizer vaccine in their pivotal trial, 127 reported serious adverse events but of these, only 3 were assessed by the investigator as being “related to investigational product”.
Selley gives the example of a healthy 49-year-old volunteer who had a myocardial infarction (heart attack) 7 days after his first Covid vaccine, yet somehow the trial investigator concluded there was “no reasonable possibility” the myocardial infarction was related to the study intervention. How could they draw such a conclusion? Pfizer agreed with this assessment refuting causality, but due to the adverse event they also excluded this volunteer from further vaccination and participation in the trial. Presumably he would be recorded as a trial exclusion for ‘protocol deviation’ (failure to receive a second vaccine), and there would be no record of his myocardial infarction in the trial summary data.
SARS-Cov2: A pandemic of publications and confirmation bias
Back in Spring 2020, when Covid-19 was considered a novel disease, clinicians began to notice a range of clinical syndromes within their various specialities which potentially correlated with SARS-Cov2 infection. This led to a deluge of published case reports and case series in the global scientific press. Even at the time, it was clear that some of these putative disease associations were tenuous at best and that in the rush to publish, quality was sometimes sacrificed to quantity.
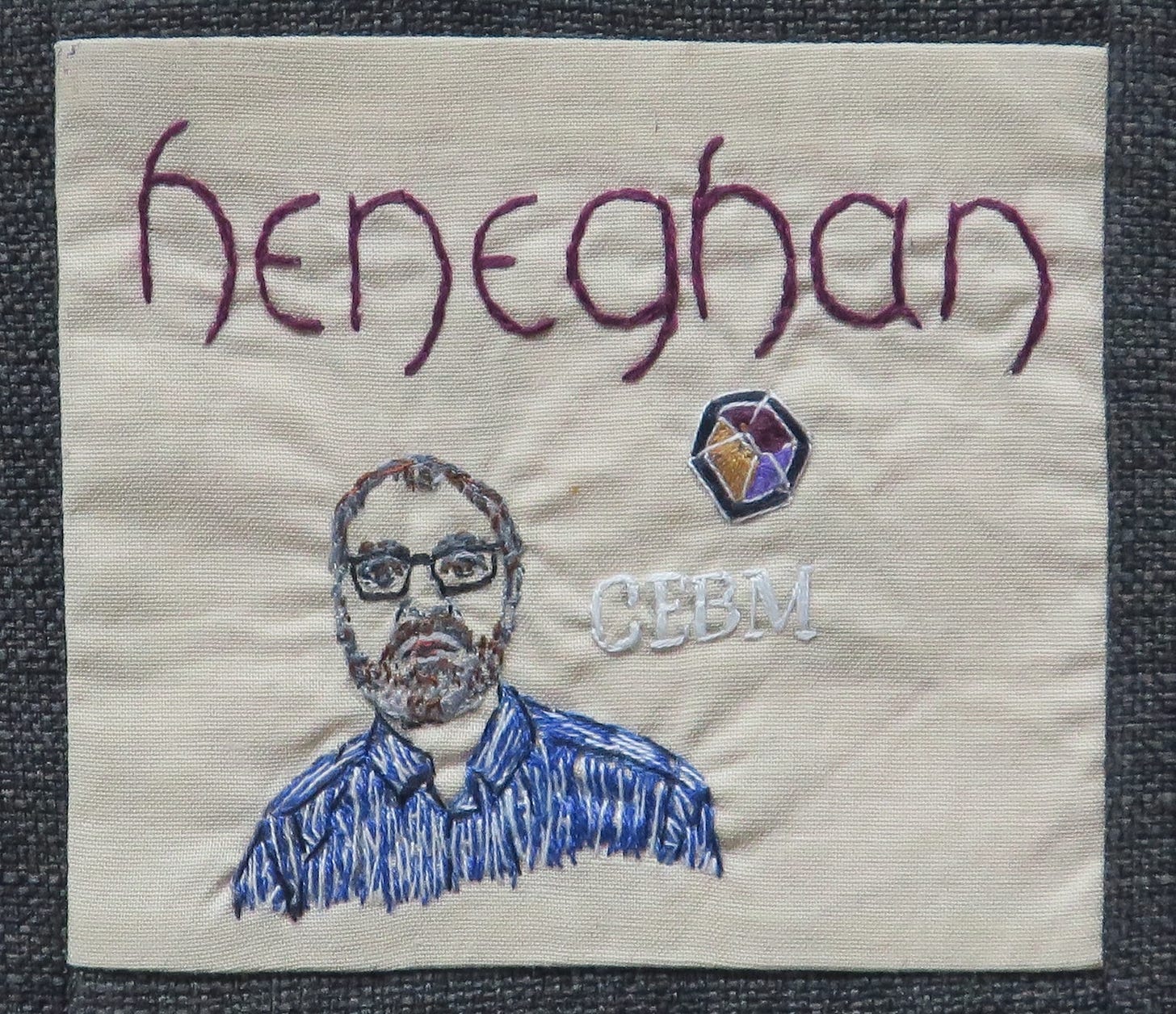
Only later, once the early panic and excitement had abated, did we start to see attempts to critically appraise the methodological quality of existing COVID-19 clinical research - much of it was poor quality. Heneghan & Jefferson refer to this era as ‘A Pandemic of Poor Quality Publications’ and in their words, ’at 377 articles a day, you’d have had to read near 16 articles an hour to keep up to date’.
Reports of Covid-19’s multi-system complications went viral in 2020, shared widely and enthusiastically in online medical forums such as med twitter. These reports would later be collated by speciality into systematic reviews, in an effort to create order from the chaos:
Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study (2020)
COVID-19-associated psychosis: A systematic review of case reports (2021)
Renal complications in COVID-19: a systematic review and meta-analysis
Dermatological manifestations associated with COVID‐19: A comprehensive review of the current knowledge (2021)
Rheumatic manifestations of COVID-19: a systematic review and meta-analysis (2020)
COVID-19-associated arthritis: an emerging new entity? (2022)
Gastrointestinal complications of coronavirus disease (Covid-19) (2021)
Cardiac manifestations in COVID‐19 patients—A systematic review (2020)
Myocarditis associated with Covid-19 disease: A systematic review of published case reports and case series (2021)
COVID-19 associated vasculitis: A systematic review of case reports and case series (2022)
A Systematic Review of SARS-CoV-2-Associated Hepatic Dysfunction and the Impact on the Clinical Outcome of COVID-19 (2022)
Hematologic disorders associated with COVID-19: a review (2021)
Urological complications of COVID-19: a systematic review (2023)
Risk of autoimmune diseases following COVID-19 and the potential protective effect from vaccination: a population-based cohort study (2023)
Medical journals appeared more reticent to publish reports of adverse events post Covid-19 vaccination, but a slow and steady trickle of similar peer-reviewed case reports post vaccination would emerge over time. These are likely to be important when making a subsequent case for causality.
Cause or Coincidence?
In the thirst to understand this new and potentially lethal virus, it was interesting to note how predisposed clinicians appeared towards uncritical acceptance of case reports as evidence of harm caused by Covid-19 infection. That is to say, causality was generally assumed until proven otherwise. It is also worth noting that when it came to reports of adverse events post Covid-19 vaccination, the opposite stance was evident and potential risks were generally downplayed.
In reality, there was often no way of knowing whether a reported disease association was actually caused by the SARS-Cov2 virus, or if it was a non-specific general complication of critical illness or treatments given, or a coincidental presentation of underlying disease, possibly unmasked by the infection or with an unrelated positive PCR test.
Nowhere was this ‘causality or confounding’ confusion more apparent than in the emergent field of ‘Long Covid’ research. Long-Covid or Post-Covid syndrome has been characterised a self-defined syndrome comprising ’symptoms persisting for more than four weeks after the first (suspected) Covid-19 infection that were not explained by something else’. By June 2021 Long Covid had amassed ‘between 170 and 205 persistent, intermittent and relapsing symptoms’. Some of these symptoms were ‘nonspecific and prevalent in the general population’, whereas others, such as ‘an inability to yawn or chapped lips’ were ‘biologically implausible, and…unlikely to meet Bradford Hill criteria for causality’. There is a risk in all this that real and significant signals are obscured by the noise. There have been calls to standardise Long Covid case-definition, with appropriate use of controls.
Similar criticisms have been directed at the growing number of reported conditions being linked to SARS-Cov2 infection. One editorial references examples of poor quality causality attribution, including ’several cases reports of encephalitis without clear evidence of central nervous system inflammation, which would not meet established definitions of the disease’. The authors ask the question, ‘how confident we can be that that SARS-CoV2 is causal in such presentations?’ They propose a systematic approach to distinguish causality from coincidence, using the 1965 Bradford Hill criteria and go on to demonstrate how this framework can be used to examine the case for causality in COVID-19 and neurological disorders.
The same criteria can be applied for establishing causality in Adverse Events Following Immunisation (AEFIs). This will be the focus of the next chapter.