Dr Iona Heath, Ex President of the RCGP, speaking at the 2021 ‘Expert Panel on Medical Mandates and Vaccine Injuries’, remarked,
‘As time goes by, theories, knowledge and certainty all come and go. The new drug that is greeted as a miracle is condemned as a poison a few months or years later.’
Given the historical track record of Big Pharma and the drug regulators, it was a wonder to behold the implicit trust they were gifted in 2021 over the novel Covid-19 gene product/vaccines. Perhaps, the uncritical acceptance of the industry claims for the vaccines reflected a desperate impatience of the medical profession and public for an inoculating weapon to enable us to ‘conquer’ the virus, quell the pandemic and find a protected route out of lockdowns. The vaccines were de facto above criticism, because globally we had invested everything - faith, reason and substance - in them. They were too big to fail the needs we had created.
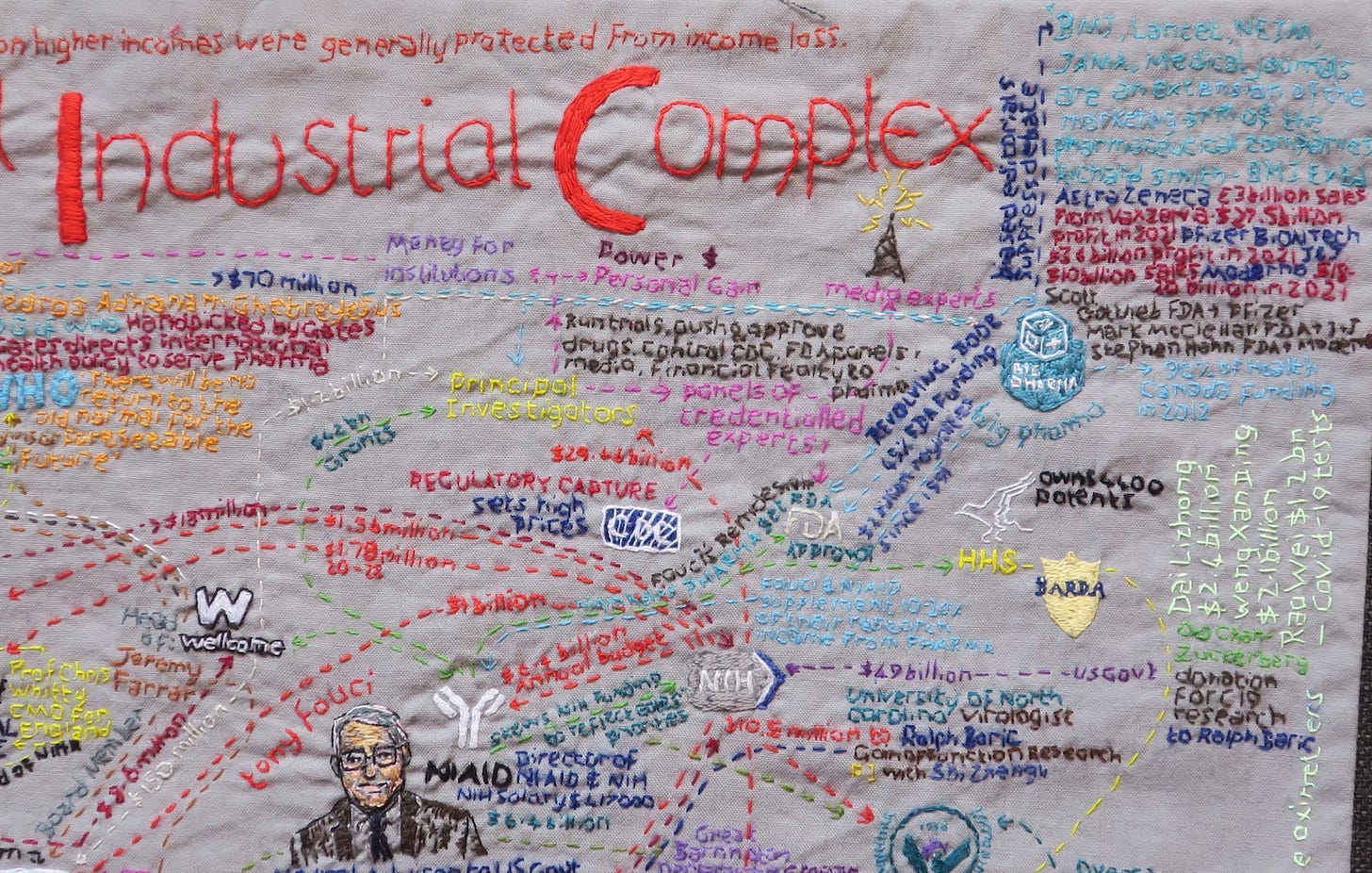
But as doctors we are expected to critically appraise evidence, and not prima facie accept industry or market vaccine claims. According to Peter Gøtzsche, ’70% of FDA scientists are not confident that products approved by the FDA are safe’ and the ‘FDA believes there is no risk that cannot be managed in the post-marketing setting’. We should therefore remain vigilant to the possibility of data suppression, regulatory capture, pervasive conflicts of interest in drug regulation and the revolving door phenomenon between politics, the drug regulators and Pharma.
History is littered with examples where the medical profession has erred in this regard (eg the Vioxx scandal), ignored signals for harm (eg Thalidomide) or succumbed too readily to group-think. Some drugs, such as Diethylstilbestrol (DES) have even caused intergenerational harms, which is to say, harm for those who do not yet exist.
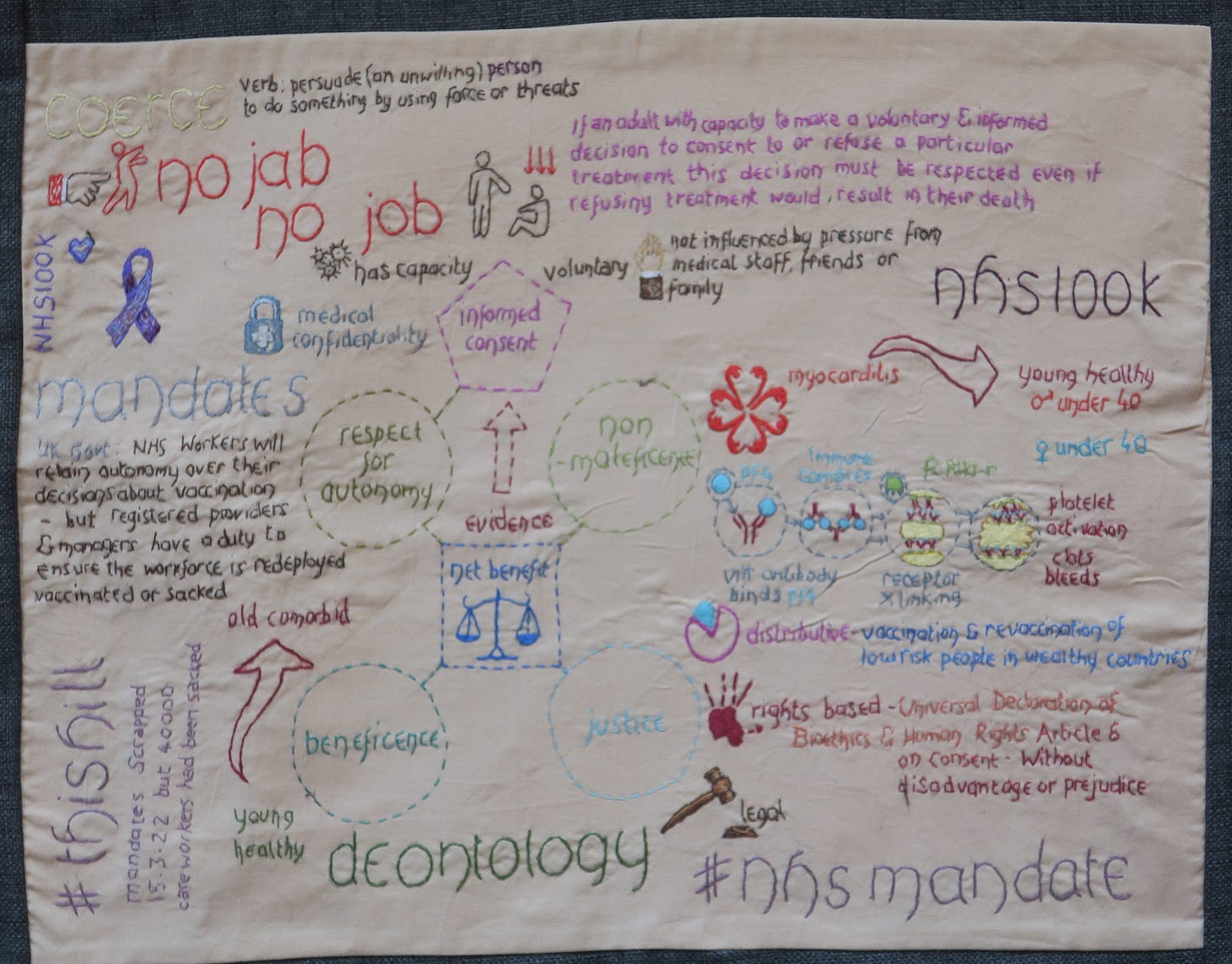
Deontology: The Four Principles Framework
The choice whether or not to take a Covid vaccination should always have been an autonomous, fully informed decision. Even more so since these are non-sterilising vaccines, so the potential vaccine benefit was always to the individual, not to the group, no matter what claims were made to the contrary.
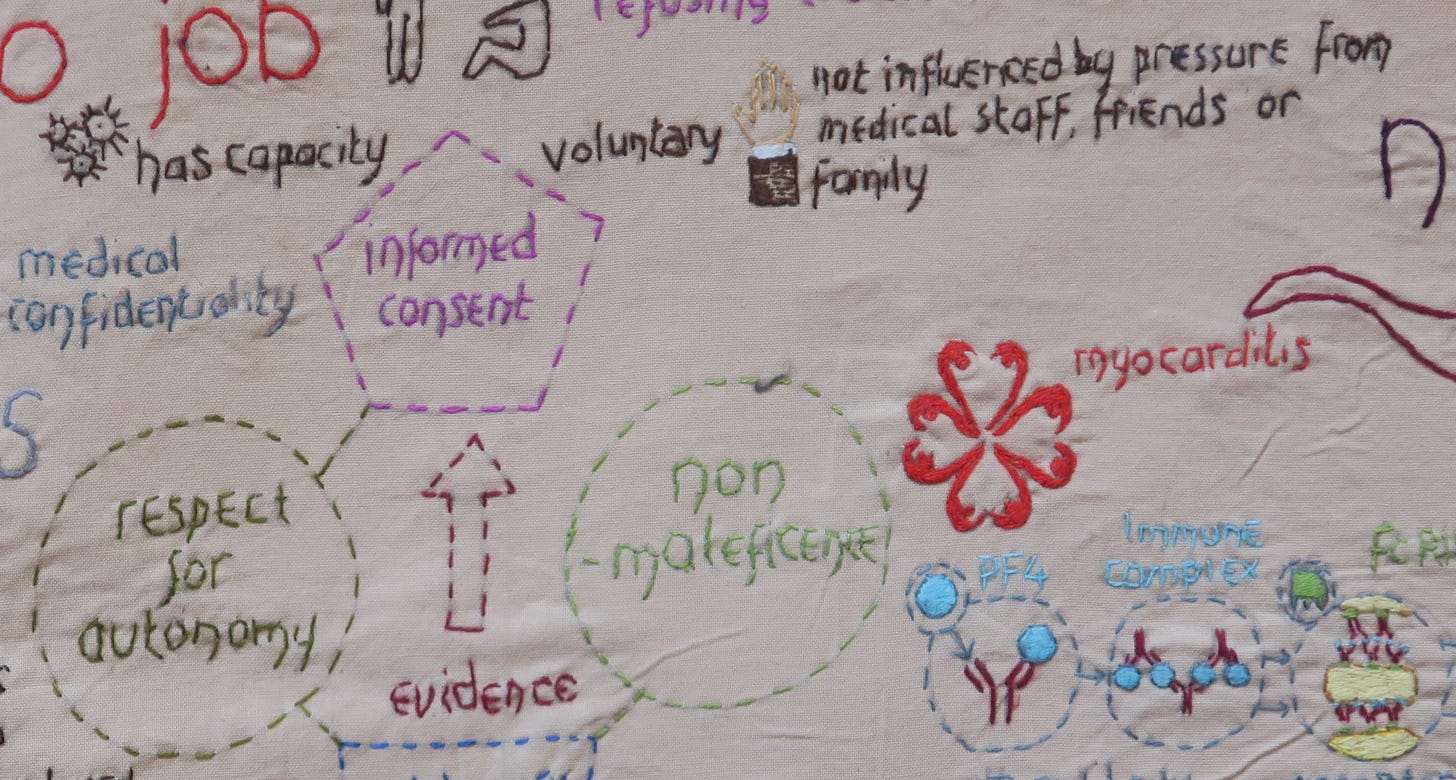
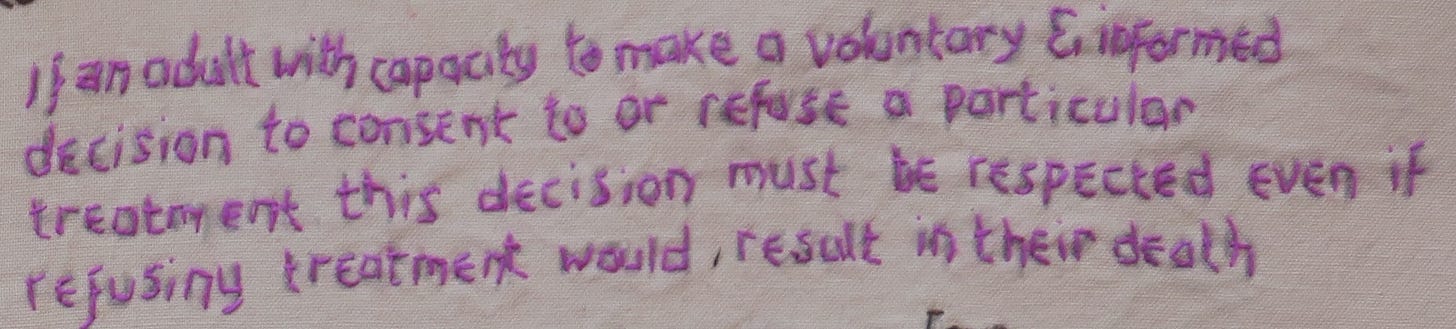
Informed consent requires adequate information, capacity to decide, and absence of coercion. Threat of loss of livelihood, as with vaccine mandates, is coercion.
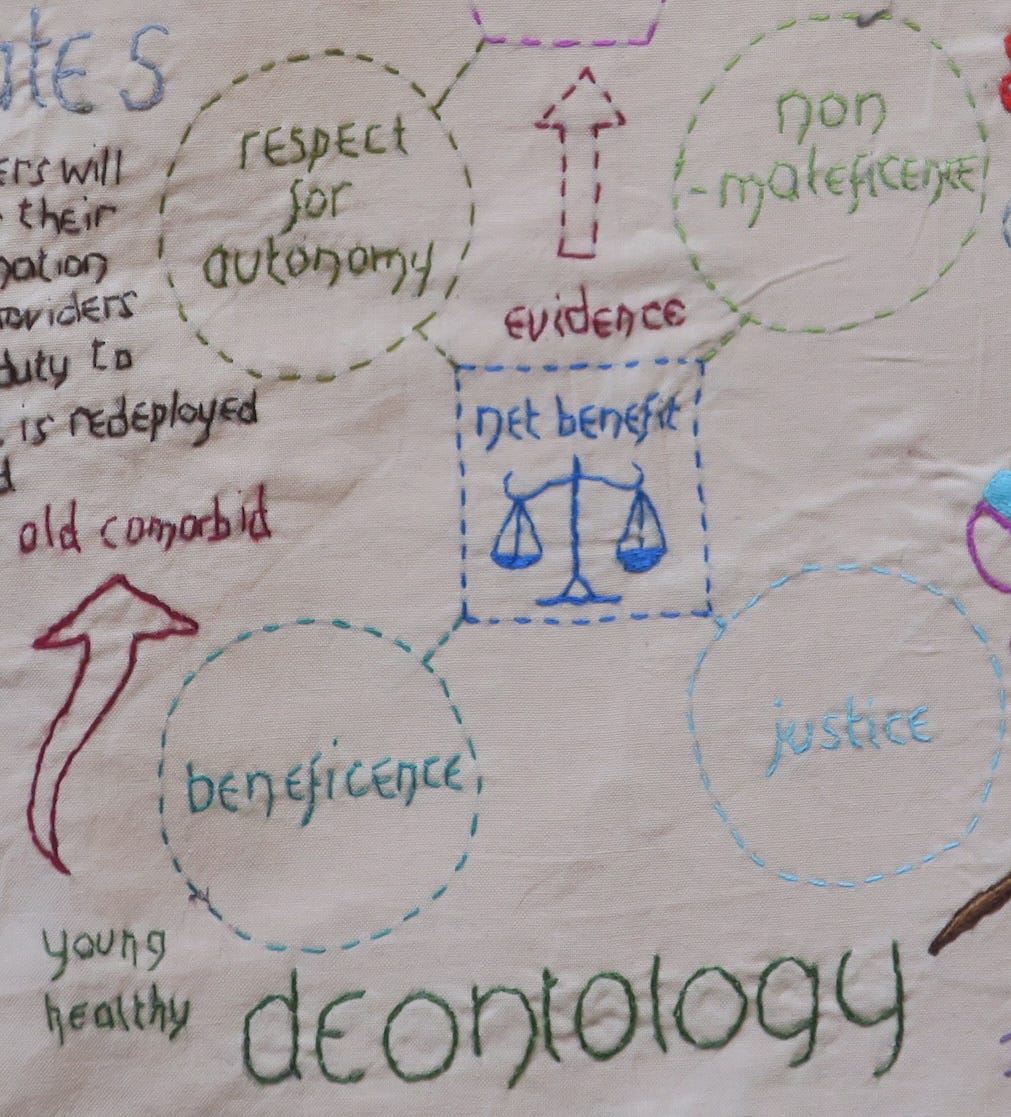
The four principles framework of Beauchamp and Childress, based on the four prima facie moral commitments to autonomy, non-maleficence, beneficence and justice assumes pivotal importance in our current approach to medical ethics. ‘Prima facie’, means that the principle is binding unless it conflicts with another moral principle - if it does we have to choose between them.
Respecting people’s autonomy and bodily integrity is at the heart of human rights and medical ethics. We help our patients make informed choices about whether to accept or decline medical treatments, by taking into consideration evidence and uncertainties about benefit and harm, and the individual’s perspective, values and preferences. NHS policy states that the decision to either consent or not to consent to treatment must be made by the person, and must not be influenced by pressure from medical staff, friends or family.
In a 1994 BMJ article, ‘Medical ethics: four principles plus attention to scope’, ethicist R Gillon expands upon this basic deontological framework:
Because all interventions carry a risk of harm, we must ‘consider the principles of beneficence and non-maleficence together and aim at producing net benefit over harm’ for each person.
Theoretically, Evidence Based Medicine (EBM) should introduce scientific rigour and so support an ethical approach to providing patient care. However, Erin Stone examines the deontological and utilitarian aspects of EBM, and cautions of the potential for biases in EBM which ‘render predictions of benefits and harms less reliable and EBM potentially less ethical’. Ethical dilemmas can arise when ‘patient values and preferences conflict with organisation-sponsored, evidence-based recommendations’. She concludes,
‘Clinicians and patients should be allowed to opt-out of a guideline recommendation (with reasons cited), and organisations should not force clinicians into ethical dilemmas in which they are caught between organisational expectations and patient values and preferences.’
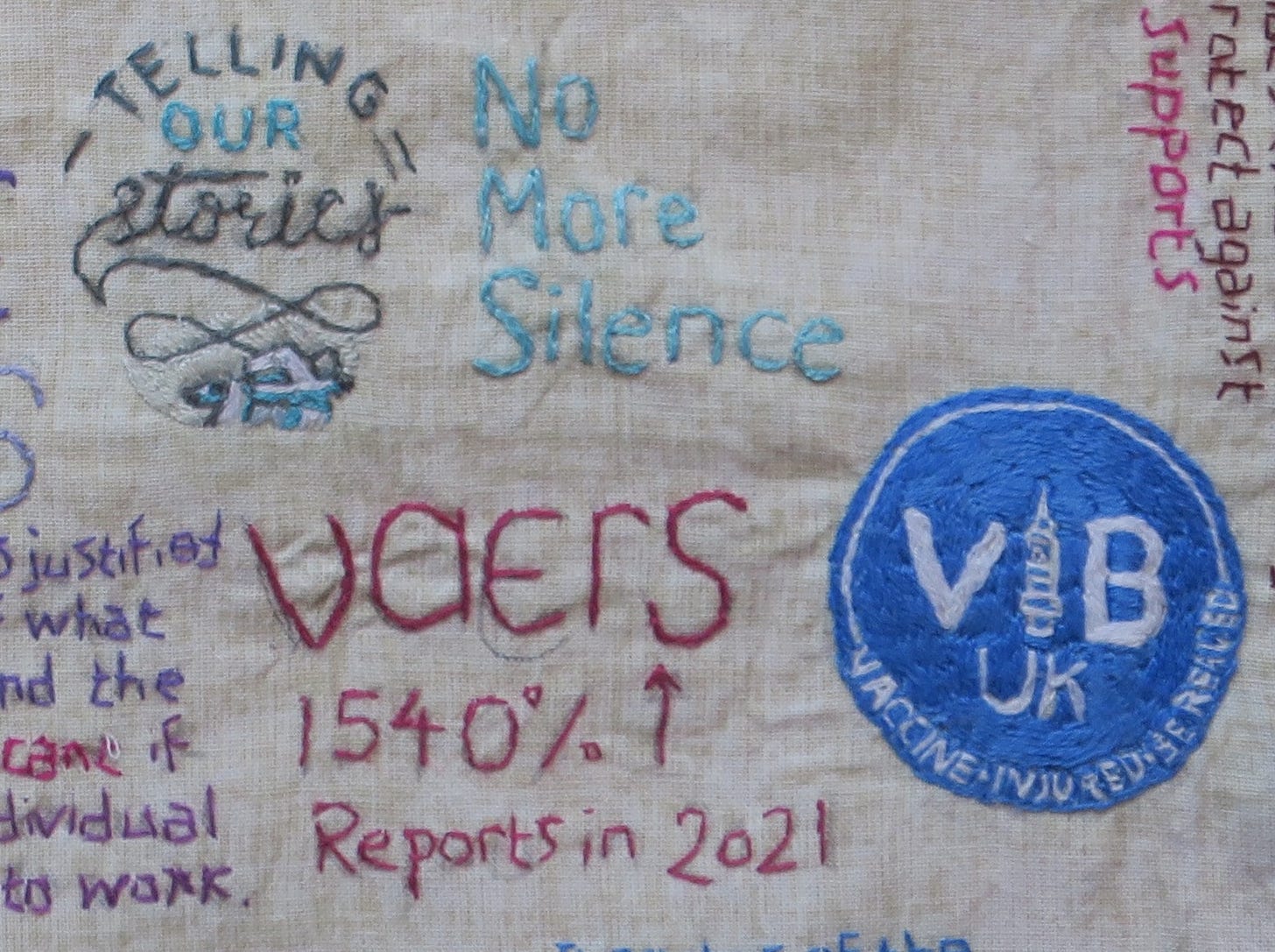
There have been strong psychological drives for our profession to dismiss, downplay, ignore and under-report potential plausible vaccine harms. In 2021, there was a belief that we could not safely be released from a perpetual cycle of lockdowns without the entire population taking a vaccine and any subsequent re-vaccinations/boosters. There was a danger that healthcare professionals could not be objective on the subject of vaccine safety if our own personal freedoms were linked to our skill in rationalising why everyone, regardless of individual susceptibility, needed persuading to take an experimental vaccine for ‘the greater good’.
To publicly raise any concern about vaccine safety is still taboo and carries a risk of professional blacklisting. To raise the concept of individual risk/benefit appraisal and autonomous choice also became taboo for a while, though this had not always been so.
We need to ‘ensure that we can provide the benefits we profess to be able to provide’.
A mandated vaccine should reasonably be expected to make a serious communicable disease significantly less ‘communicable’. This benefit should endure for more than a couple of months. Though we now talk about waning immunity and annual boosters as if that had always been on the cards, you only have to look back to see what scientists, politicians and pharmaceutical companies were predicting in Spring 2021, to see that this was not the case.
In February 2021 we were told we needed about 80% coverage for the NHS vaccination programme to be successful, to achieve herd immunity. We were told that vaccines were 100% effective against hospitalisation and death, that when infections do (rarely) occur, vaccinated people are almost always asymptomatic, don’t carry the virus, don’t get sick and don’t pass it on; they are dead ends to the virus and breakthrough infections very very rare.
In April 2021, after an aggressive early vaccination campaign, Israel thought they had achieved herd immunity but by August their cases started rising and third doses were given.
To those playing close attention, it became clear early on that the hopes and expectations for these vaccines - that they would lead to sterilising and herd immunity - were not being borne out and that we do not really know how the virus may evolve in a global mass vaccination environment.
We must respect the patient's autonomy for what constitutes benefit for one patient may be harm for another.
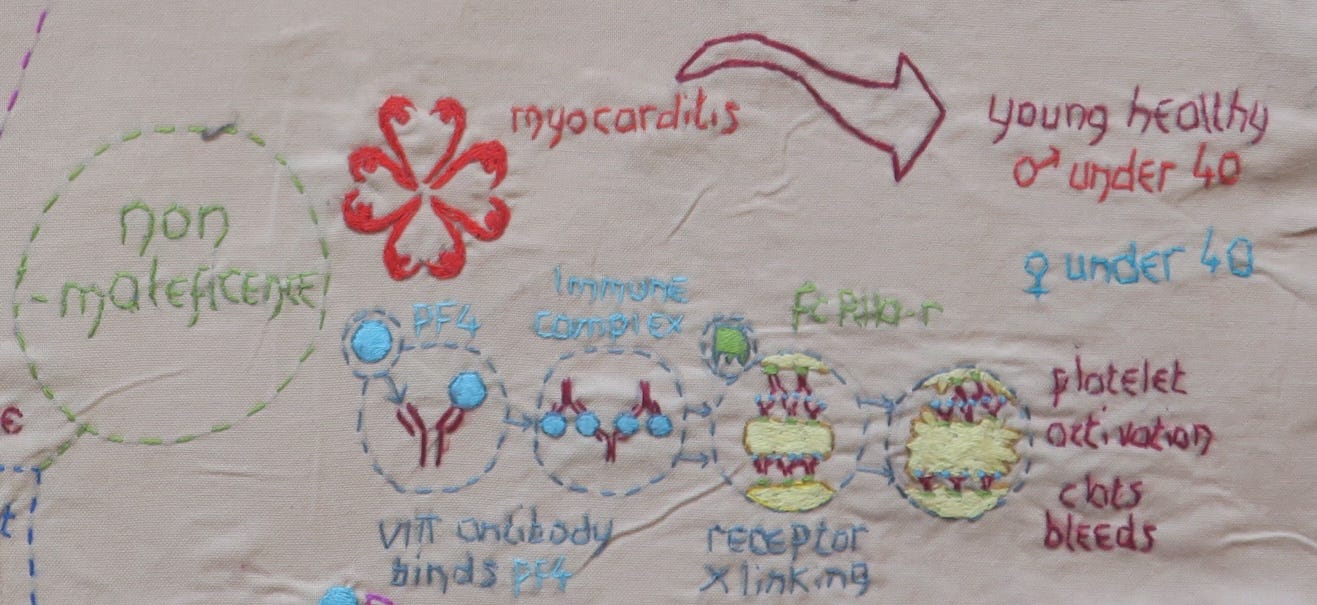
Benefits and Harms of the novel vaccines were always unequally distributed. Not everyone had a predicted net benefit, especially healthy people under 50 years of age.
The obligation to provide net benefit to patients requires us to be clear about risk and probability when we make our assessments of harm and benefit.
In November 2020, the GMC updated its guidance on consent:
“You should usually include the following information when discussing benefits and harms…any risk of serious harm, however unlikely it is to occur.”
replaces the 2008 wording,
“You must give patients the information they want or need about…the potential benefits, risks and burdens, and the likelihood of success, for each option.”
For informed consent we needed up-to-date information, better tools for risk communication and honest transparency about unknowns. Instead, we saw individual risk of vaccine injury contextualised by drawing comparison with pooled risk from Covid-19 infection, or risks stratified by age, but not by co-morbidities. The few risk charts we were given focussed only on one specific risk, but vaccine-related risks can be multiple and varied.
Despite people stating they value the ethical principles of beneficence, non-maleficence, respect for autonomy and justice, research demonstrates that they do not always actually use these principles directly in the decision-making process. Other ‘situational factors’ and ‘situational information’ assumes greater importance in ‘re-weighting’ principles. If the 4 principles are not actually used in decision-making by clinicians then it raises questions about their overall utility and applicability.
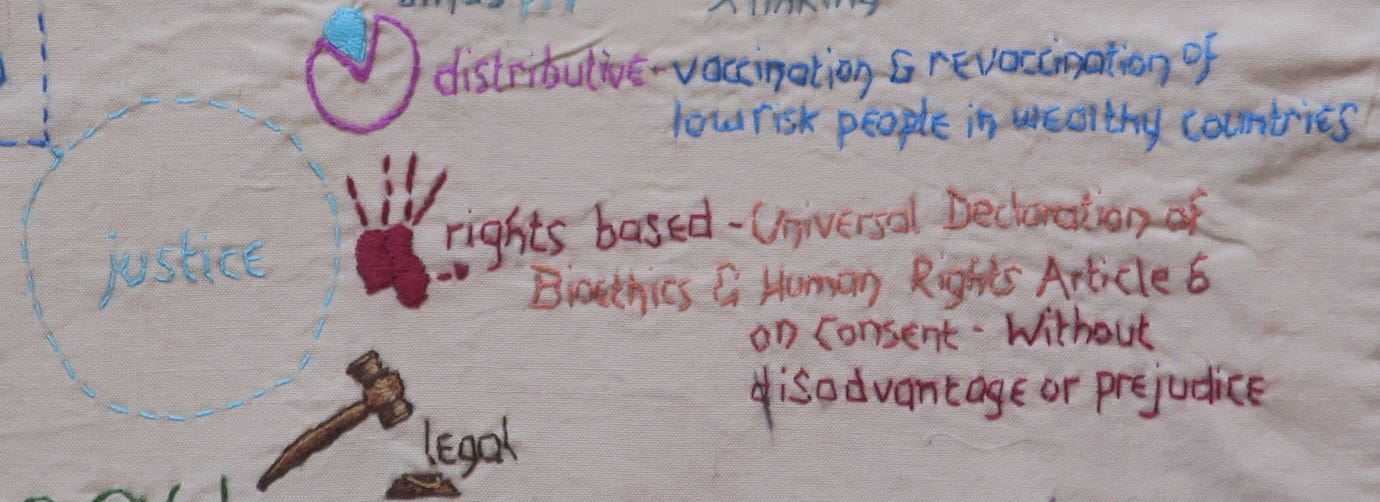
Many argue that in presenting the public with biased or incomplete data and pooled risk analyses, by vaccinating people at low risk from Covid-19 infection when the long term consequences of mass vaccination are unknown, and by over-selling vaccine effectiveness, we denied people their right to informed consent.
Utilitarianism
The right to autonomy and consent has never been considered absolute. Using the principles of capacity and justice towards other individuals, the right to autonomy has been cut in a few well-defined circumstances. The Public Health (Control of Disease) Act (1984) regulates notification of diseases and mandatory treatment of conditions like TB - here the individual’s right to consent is severely restricted.
In the 2020 updated GMC guidance, we now see public health and mental health legislation lumped together in one paragraph:
’A patient’s right to make a healthcare decision for themselves can be affected by mental health or other** legislation and by common law powers of the courts. Patients may be required by law to comply with assessment or treatment because they present a risk to themselves, to their health or to others.’
(**For example, the Public Health (Control of Disease) Act 1984; the Public Health etc. (Scotland) Act 2008; the Public Health Act (Northern Ireland) 1967)
Utilitarian philosopher John Stuart Mill stressed an individual’s right to autonomy should only be restricted in exceptional circumstances,
“the only purpose for which power can be rightfully exercised over any member of a civilised community, against his will, is to prevent harm to others. His own good, either physical or moral, is not a sufficient warrant. He cannot rightfully be compelled to do or forbear because it will be better for him to do so, because it will make him happier, because, in the opinion of others to do so would be wise, or even right”.
Some see it as justified to restrict a person’s freedom to make an autonomous choice to decline vaccination, when the following conditions are met:
Vaccines are safe and the costs believed to be small.
Vaccines are effective in blocking transmission, meaningfully contribute to population immunity and prevent significant harms.
Less intrusive measures on individual freedom have not worked.
In 2021, a minority of healthcare professionals came to believe that the threshold for universal SARS-Cov2 vaccine and vaccine mandates had been reached. Nevertheless, it remains an uncomfortable truth that if everyone is made to take a vaccine, some will be harmed by the vaccine, including people who would not have personally benefited from the intervention. For those who believe in the righteousness of universal vaccination, this is seen as an acceptable sacrifice or trade-off, because they believe there is a net benefit to the population.
Even so, clinicians who believe in mandates would balk at personally coercing someone to take a medical treatment that they do not want or need. Those clinicians might also fear being held accountable if the person ubsequently came to harm.
Arguments for universal SARS-Cov2 vaccination of healthcare workers were undermined by a number of factors:
Mandates were based on a misrepresentation of evidence for safety and efficacy, that is to say, benefits were oversold and harms have been downplayed.
The evidence presented for vaccines has been subject to organisational and drug-industry sponsored bias. There are many scientific, medical and political conflicts of interest.
Political decisions on mandates were made too early, in what was a dynamic situation, based on snapshots of vaccine effectiveness and flawed modelling using wrong assumptions. This led to wrong conclusions being drawn about the potential impact that mandates would have had on viral spread and on staff sickness.
The impact of mass vaccination on virus ecology was not considered. Mass vaccination with ‘leaky’ products that provide only partial immunity, during an active epidemic of a mutable virus, may selectively drive the dominance of more infectious variants, ultimately leading to vaccine resistance and the call for yet more vaccine production and distribution.
Proportionality: Covid vaccine mandates, with ensuing job losses, would not be considered proportional once the virus is generally accepted to be on a par with the common cold.
Loss of objectivity: Decisions on mandates were made because people believed in the lockdown-vaccination suppression strategy and could think of no other way of exiting self-imposed lockdowns without experiencing mass cognitive dissonance.
No impact assessment was made on how losing tens of thousands of workers would affect a health and social care service already at breaking point due to political choices made over decades by successive governments.
Covid vaccine mandates and threats of mandates leads to a loss of valued health and social care workers from the workforce. This adversely affects everyone who works in or uses these services, irrespective of a their voiced or unvoiced opinions about the rightness or wrongness of medical mandates, to say nothing of the imponderable loss of a varied group of individuals of probity or conviction in relation to human medical treatment.




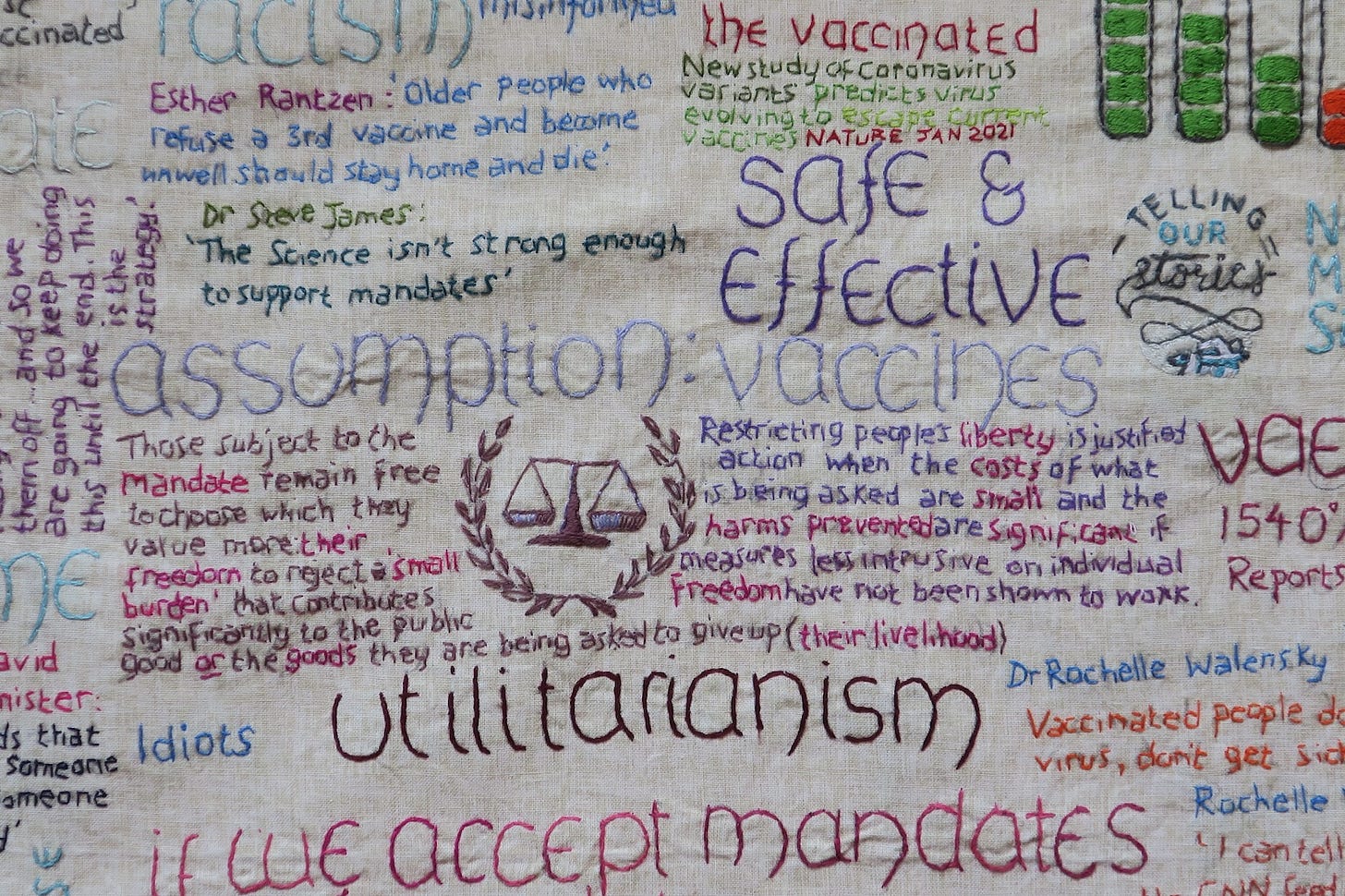
I never understood how they could say ‘safe and effective’ for a novel therapy without long-term safety data.
On top of that a large cohort of the population was never in danger of severe disease or death from this virus.
Geert Vandenbossche warned that vaccinating the population out of a pandemic was never a good idea and would not achieve herd immunity.
In previous lives these products would have been taken off the market long ago.
The chikungunya vaccine was pulled when 3 people developed signs of arthritis in the trial.
So now we have a PM who today in Parliament says that ‘Covid vaccines are safe’, whilst we now know there are known issues, such as the potential for cardiac problems, DNA contamination, frame shifting and the question of all the potential causes of the excess deaths in multiple countries.
I have just ordered Julie Ponesse’s book ‘My choice’, a Canadian ethics professor who resigned in tears when she could not go along with the mandates and continue to teach ethics.
It is my opinion that these mRNA products should be pulled off the market whilst further analysis of data is carried out.
Good news is that people are voting with their feet.